My Suprapubic Catheter Surgery
Eight months ago, my Urologist suggested I get a suprapubic catheter (SPC) to improve my quality of life. Due to my Ehlers-Danlos Syndrome (EDS), I have numerous urological issues including an overactive bladder, urgency and retention, recurring Urinary Tract Infections (UTIs) and pain caused by over-zealous mast cells in my bladder wall. Despite the problems my EDS causes with surgery and healing, I agreed and began counting down the days until my procedure.
It Was Time For My Bladder To Retire
To complicate things, I tested positive for MRSA before my procedure. It was ‘colonising’ which meant the bacteria was sitting on my skin and, although not causing harm, there was now a risk of developing an actual MRSA infection from the surgery. I spent four days scrubbing myself in the shower and rubbing special cream in my nose to try to kill off the bacteria.
My surgeon visited me on the morning of the big event and explained what would happen plus any risks involved. He described how the bladder sits behind the pubic bone so he would fill it with fluid to make it rise up in order to get the catheter into the best place. I went to the toilet for the final time and thanked Dennis, my troublesome bladder, for his loyal service.
The surgery went well. The first thing I said to my wife when I woke up was “I don’t need a wee!” She was hoping for “I love you” - but after two years of constantly feeling like I was ready to burst, my overriding thought was how amazing it was to feel my bladder finally relax. Still a little dazed from the anaesthetic, I took a peek at my new tube and was surprised to see what looked like a dishcloth stuck to my ‘personal space’. The bright blue dressing was hugging my catheter, which I aptly named JCB - Jay Cloth Boris.
It Took A Little Time To Get Used To My New Bladder Buddy
It took a few days to get used to my suprapubic catheter (SPC). I bought a padded tote bag, which could hang on my wheelchair, to carry my urine bag in.
It took a few attempts to work out the best way to place the newest addition to my medical tube collection in bed but I looked forward to bedtime for the first time in years. Once I was tucked up in bed, I knew I could relax as I wouldn’t be getting up for a wee every few minutes. On the third day, I realised I hadn’t even thought about going to the toilet. In the past I had to remember to self-catheterise every few hours because I could retain a lot of urine. I was over the moon with my new SPC and was already feeling the benefits.
Not Everything Went Smoothly
The main reason I got my SPC was so I would not be in pain and feel like I need the toilet whenever I lie down. Unfortunately I do still have this issue. Some nights my catheter rubs on my bladder wall giving the sensation of needing the toilet. Other nights it digs into the bottom of my bladder due to my small size and wonky insides. This can be quite painful, especially when I lie on my back. If I lie on my side, the awkward position of the stoma means it doesn’t drain well. Sadly I am in just as much discomfort in bed now as I was before my SPC.
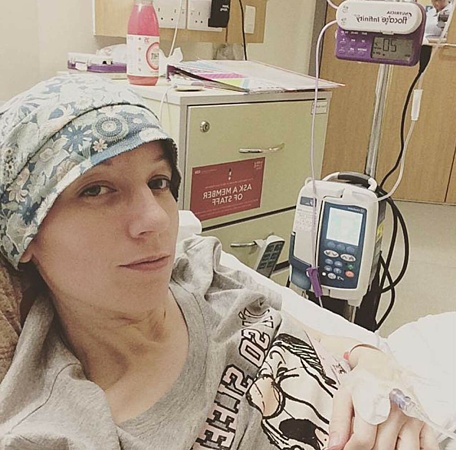
Despite carrying out the preventative treatment to clear my skin of MRSA bacteria, I was unlucky that it still managed to get into my catheter site. I woke up one day in a great deal of pain and went straight to hospital where my site was swabbed for MRSA. Blood tests showed I had an infection so I was given a course of antibiotics and the swab confirmed MRSA. The infection got quite bad and I became ill quickly. I slept all day and was too exhausted to get out of bed. The pain was bad and I questioned whether it had been worth it. How was this improving my quality of life?
It Was Worth It In The End
But now the infection is clearing and, despite the difficulties, I am still glad that I had the procedure done. The infection will clear and there are some options to help reduce the discomfort of the catheter inside my bladder. I don’t spend all night back and forth to the toilet anymore so I am no longer dreading going to bed. Car journeys aren’t spent crossing my legs desperately looking for a public toilet every ten minutes. I no longer have to self-catheterise, causing pain to my heavily damaged urethra.
I’m still trying to find the right urine bag for my needs and I’m a bit scared about my first catheter change but, overall, I am really thankful for my suprapubic catheter.
Getting a suprapubic catheter can improve quality of life
Carrie tried leg bags instead of night bags - see her experience here
Share this article:
by Carrie Beckwith Fellows



About the author
Hi I'm Carrie, I live in rural Northumberland. I have complex health issues including severe intestinal dysmotility and bladder dysfunction caused by Ehlers Danlos Syndrome. You can follow my blog at www.ruralteacake.com.



